“Opt-Out” HIV Testing: A Better Paradigm in the Real World
Twenty-five years ago, the disease we know as HIV/AIDS was thought to affect only gay men, and consequently was relegated to the back benches of medical treatment, understanding, and constructive discussion. Little was known about the emerging epidemic, and many coped with the implications of their sickness in relative silence. With no treatment options available, there was little hope for people testing positive for HIV.
Much has changed since then.
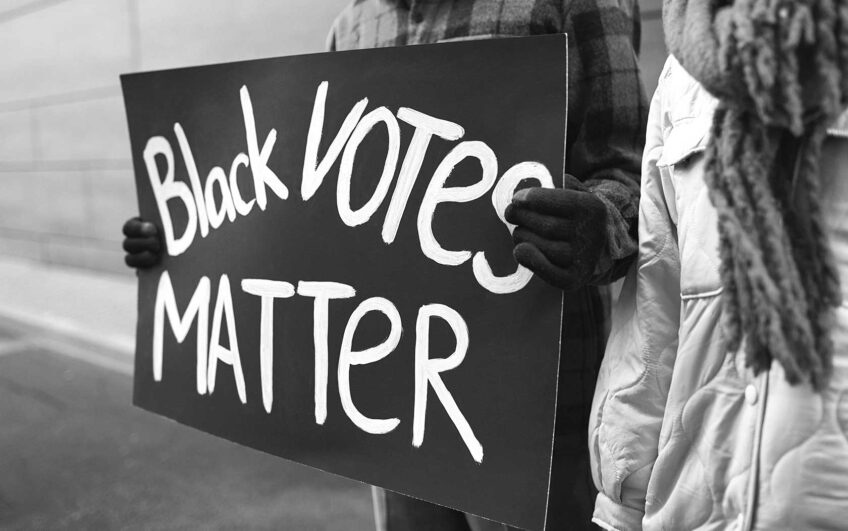
Today, advances in treatment have led to HIV/AIDS being a chronic disease rather than the death sentence of years past. The face of HIV/AIDS has changed as well. Unlike 25 years ago, Black and Latino residents now account for more than 50 percent of all persons living with HIV in Massachusetts, even though they make up only 12 percent of the state’s population. Roughly 70 percent of all cases of HIV among women are found among Black and Latina women, who are much less likely than men to know they are at risk for infection.
The need for improved strategies to stop new HIV infections is urgent.
The U.S. Centers for Disease Control (CDC) estimates that 21% of people infected with HIV do not know they have the virus. That means over 5000 people in Massachusetts are living with undiagnosed HIV. Because they have not been tested and connected to medical care, many are unwittingly transmitting HIV. Up to 70% of new infections occur because individuals are unaware of their HIV status. Yet, studies show that when people know they are infected, they are less likely to transmit the virus to others.
Sadly, the longer you wait to learn you have HIV, the more you limit your chances of effectively treating the disease. In 2006, in the 34 states where such information was available, 36% of new HIV infections were subsequently diagnosed with AIDS within 12 months. In Massachusetts, the proportion was notably higher — 42%. These statistics demonstrate how delayed testing leads to late entrance into care, which in turn results in lives cut short.
The evidence is compelling: we must bring renewed vigilance to the fight against the continued spread of HIV/AIDS. One proven method for reaching more undiagnosed individuals is for all health care settings to adopt what is known as voluntary “opt-out” HIV testing. It is the approach recommended by the Centers for Disease Control and Prevention (CDC).
Fortunately, there is now consensus among a broad cross-section of stakeholders that the Commonwealth’s HIV testing laws must be modernized to ensure that more people are tested. While current Massachusetts HIV testing law does not allow for “opt-out” testing, change now appears to be on the way. And in light of more than 5000 individuals statewide who do not know they are infected with HIV, doing nothing would be a reckless deferral of action.
For twenty-five years, patients in Massachusetts have been required to “opt-in” to an HIV test, by giving their separate and specific written consent before a doctor can conduct the test, a standard required for no other medical test. However, the state Legislature is now considering a bill that would make HIV testing similar to any other health screening that patients receive after signing a standard “general consent” form for medical care. Under Senate Bill 821, a patient will be informed about the HIV test before being tested by their physician, and will still have an opportunity to “opt-out” and decline the test. The bill maintains the strong existing privacy protections related to disclosure of an individual’s health status, as well as stiff penalties for anyone who violates them.
The movement from an “opt-in” to an “opt-out” system may sound like a mere change in terminology. But as a practical matter, it can sometimes make all the difference in the world. Studies have shown that “opt-out” approaches to screening in other health areas have increased detection of illness. If successful, the change will be welcomed and long overdue.
With “opt-out” testing, an HIV test will become a standard procedure during a routine medical visit. Providers will be more likely to test for HIV, advancing the CDC’s goal of reducing the number of new infections and offering medical care to persons with HIV as early as possible.
The current HIV testing system is a barrier to linking those living with undiagnosed HIV to care, and it must be changed. But any change in HIV/AIDS policy must be done right. To reach the 5000-plus residents who are unaware of their status, and to stem the tide of HIV transmission, Massachusetts must embrace an “opt-out” model.
Gary Daffin is the Executive Director of the Multicultural AIDS Coalition in Boston and serves as a Co-Chair of the Prevent AIDS Now Coalition.
Dr. Laura Kogelman is the Director of the Infectious Disease Clinic at Tufts Medical Center.