Health centers see influx of patients, longer wait times since Carney closure

When the announcement came that Dorchester’s Carney Hospital was set to close on an expedited, 36-day timeline, community members expressed concerns that the loss of the neighborhood’s only hospital would increase the burden on surrounding health organizations and increase the time it takes for patients to access care.
Now, about a month after the hospital closed its doors on Aug. 31, many of those predictions are coming to pass, even as state and local organizations work to close gaps.
That closure of Carney Hospital came following a declaration of bankruptcy from Steward Health Care, which owned Carney Hospital, in May.
While the for-profit health care company was able to strike deals in a Dallas-based bankruptcy court for the sale of five of its Massachusetts hospitals, the court determined that there were no qualified bidders for Carney Hospital or for Nashoba Valley Medical Center in Ayer, and both hospitals were shuttered at the end of August. Steward CEO Ralph de la Torre announced Saturday that he was stepping down after failing to testify before a Senate panel.
In four of the sales — those of Good Samaritan Medical Center in Brockton, Holy Family Hospital in Methuen and Haverhill, Morton Hospital in Taunton and St. Anne’s Hospital in Fall River — agreements to sell each hospital’s real estate and operations were agreed on.
However, for the fifth hospital — St. Elizabeth’s Medical Center in Brighton — Steward agreed to transfer operations of the hospital, but sale of the land was blocked by asset management firm Apollo. Steward had sold the hospital’s land to Apollo in 2016.
On Sept. 27, the Healey-Driscoll Administration announced it had officially seized the land at St. Elizabeth’s through eminent domain to facilitate the transfer of operations to Boston Medical Center, who agreed to purchase the hospital.
But for communities in and around Dorchester previously served by Carney, much of the impact that local organizations were bracing for with the closure appears to be panning out. At the nearby Codman Square Health Center, leadership was expecting an increased number of patients at the center’s urgent care and heightened severity of what those patients need.
Both expectations have so far come true.
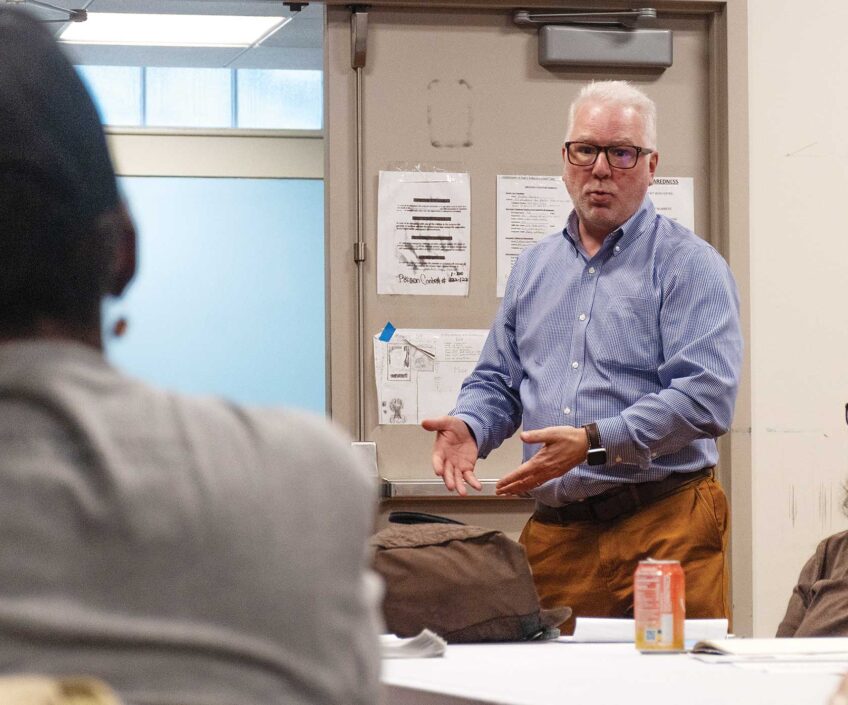
“Sicker patients means more time you need to spend, which means you have longer wait times in the waiting room,” said Dr. Guy Fish, the center’s CEO.
Previously, Fish, who stepped into the center’s top role in August, said the center saw about 75 patients per day in its urgent care, with an uptick to about 100 on Mondays due to pent-up demand as the facility isn’t open on Sundays. Now, he said, Codman Square Health Center is regularly seeing 100 patients on Tuesdays, and often increased numbers on Wednesdays as well.
Despite early preparation, the closure hit especially hard at first, and Codman’s urgent care saw wait times rise to five hours — Fish said those are back down to about two hours now.
In response, the health center shifted its triage center, which used to operate behind the scenes, into the front of the facility, setting up computers and screens for privacy in a quick change over two or three days, Fish said.
And the health center started more aggressively looking to fill open positions — Fish said they’re still looking for one more provider at the MD or nurse practitioner level. They’re changes that, without broader shifts in the health care ecosystem, Fish said, will probably be around long-term.
“I think the perspective that we have is that these changes of bringing triage out front and staffing are likely to be permanent,” Fish said. “We are looking at this on a week-by-week basis to make that determination.”
Michael Curry, president and CEO of the Massachusetts League of Community Health Centers, said that impact has been felt at health centers across the area. Those same centers, he said, have also identified challenges where would-be patients show up at the facility only to find it shuttered with no clear communication about where else they can go.
Still, despite the uptick in need that the health center has identified, Fish said leadership at Codman Square Health Center suspects that some of the patients who would have gone to Carney Hospital’s emergency department for care are postponing or just not getting the care they need.
“One of our big concerns is that we have a belief that more medical care need is in the community than we’re seeing, but that patients who would readily go to Carney are maybe deferring care due to barriers to care such as transportation or not knowing where to go,” he said. “That means that when patients do show up, they’re often sicker and more expensive to get back to good health.”
He said Codman Square Health Center hopes to partner with other institutions to improve messaging and efforts to avoid delays in care.
Emergency care from Boston Emergency Medical Services and surrounding hospitals has also seen an uptick in need.
Beth Isreal Deaconess Hospital Milton — the nearest emergency department at about two miles from Carney’s now-shuttered facility — has seen an impact from the closure of Carney’s emergency services, said Kristina Murray, a spokesperson for the hospital.
“We have taken steps to prepare for any increase in volume and our priority is ensuring uninterrupted care for any patients in need. We have seen an increase in patients who previously used Carney Hospital, and we are closely monitoring the situation as it evolves,” she said in a statement.
For the city’s EMS department, which is run through the Public Health Commission, spokesperson Caitlin McLaughlin said they’ve seen some increase in transport times to hospitals— up about 1.8 minutes from the same time last year — but a small reduction in response times — about 0.3 minutes — since Carney Hospital closed.
To account for the anticipated uptick in need, Boston EMS has assigned an extra ambulance to Dorchester to boost coverage, she said. That is in addition to the department’s Paramedic 3 Ambulance, which has, for more than 20 years, operated out of a bay at Carney Hospital. Despite the facility’s closing, the ambulance continues to run from the same location, McLaughlin said — an element that had been in question ahead of the closure.
“Our priority is to ensure all patients continue to receive the prehospital care that they need, regardless of where in the city services are required,” McLaughlin said in a statement.
The state government is looking to identify new ways to fill gaps as well. On Sept. 25, the Healey-Driscoll administration announced a Dorchester-based working group to stabilize and revitalize care in the area surrounding Carney Hospital — as well as a similar group in Ayer looking to address needs following the closure of Steward’s Nashoba Valley Medical Center there.
The Carney-focused group will be co-chaired by Curry, from the Massachusetts League of Community Health Centers, and Bisola Ojikutu, executive director of the Boston Public Health Commission.
“The focus that we’ll have is to look at impact of this closure in Dorchester, what it means for access to emergency services, to urgent care, specialty care, to behavioral health services,” Curry said in an interview. “What does the destabilization mean for patients, for workers and for the community?”
Over a three-month period, the group will convene a collection of community leaders and city and state officials, selected in conjunction by Curry and Ojikutu as co-chairs as well as the Healey-Driscoll administration and the Mayor’s Office, to look at what the impacts of the closure are and how care can shift to accommodate those gaps.
In that work, Curry said it will be important to make sure existing health disparities aren’t worsened. Data from the Boston Public Health Commission have identified neighborhoods like Roxbury, Dorchester and Mattapan as suffering from worse rates of conditions like cardiometabolic diseases, preventable cancers, and opioid overdoses.
“We can’t let this closure exacerbate those conditions and those outcomes,” Curry said. “The purpose of this report and the work that we’ll do over the next three months is to figure out a way to address the inequities and the feared outcomes of a closure on the most vulnerable among us in the most vulnerable communities.”
Part of that might mean increasing resources to community health centers, the leaders of which Curry said will be part of the task force. He expects those leaders to advocate for increased support as they grapple with heightened need and increased severity of patients showing up.
Other political and community leaders quoted in the release framed the working groups as an opportunity to reimagine and innovate.
“We’re going to bring together community and industry leaders to develop a game plan to not only protect but improve health care in the regions most impacted by Steward’s greed and mismanagement,” Gov. Maura Healey said in the release.
Boston Mayor Michelle Wu called it “should be a process that strengthens access to care for Boston residents.”
Fish, too, said he hopes that effort can think outside the box, pointing to options like “hospital at home,” where patients who need an acute level of care can, instead of going to receive that care in a hospital, get monitoring and nursing from their own home instead.
The American Hospital Association has said that model can reduce costs, improve outcomes and enhance the patient experience.,
“Hopefully those teams will be able to think out of the box, not in terms of necessarily there being hospitals that need to operate in an 1800s model of community hospitals, but with a more modern understanding of what medical needs there are in communities, what health needs there are communities in a progressive way that looks upstream to keep a focus on wellness, particularly behavioral health and prevention,” Fish said.